shoulder examination pdf
Shoulder Examination⁚ A Comprehensive Guide
This guide provides a structured approach to shoulder examination, encompassing initial assessment, inspection, palpation, range of motion analysis, and various provocative tests for impingement, rotator cuff, labral tears, instability, and biceps pathology. Neurological examination and imaging considerations are also included, culminating in differential diagnosis and documentation.
I. Initial Assessment and History
The initial assessment begins with a thorough patient history. Key questions should ascertain the onset, location, and character of the pain. Is it sharp, dull, aching, or burning? Does it radiate? The patient should describe the mechanism of injury, if any, including specific activities or events that precipitated the symptoms. Relevant past medical history, including previous shoulder injuries, surgeries, or systemic illnesses, should be documented. Current medications, particularly those affecting inflammation or pain, should be noted. The impact of the pain on daily activities, including work, sleep, and leisure pursuits, should be explored. The patient’s occupation and hobbies are crucial as they can provide insight into repetitive movements or overuse that may contribute to the condition. Finally, inquire about any associated symptoms, such as weakness, numbness, or tingling. This comprehensive history provides a foundation for targeted physical examination.
II. Inspection and Palpation
Visual inspection of the shoulder begins with a comparison of both shoulders, noting any asymmetry in posture, muscle bulk, or bony landmarks. Observe for any signs of swelling, discoloration, deformity, or scarring. Assess the patient’s posture, looking for signs of scapular dyskinesis, such as winging or elevation. Palpation follows, systematically assessing bony structures. Begin with the acromioclavicular joint, feeling for tenderness, crepitus, or step-off deformities. Palpate the coracoid process, then the bicipital groove, checking for tenderness along the biceps tendon. Examine the greater and lesser tuberosities of the humerus, assessing for any irregularities or tenderness. Palpate the surrounding musculature, including the deltoids, rotator cuff muscles (supraspinatus, infraspinatus, teres minor, and subscapularis), and the trapezius, noting any muscle spasms, tenderness, or atrophy. Gentle palpation of the glenohumeral joint line, both anteriorly and posteriorly, should also be performed. This systematic approach allows for identification of focal tenderness and abnormalities suggestive of specific pathologies.
III. Range of Motion Assessment
Active range of motion (AROM) assessment begins by observing the patient performing shoulder movements. Assess flexion, extension, abduction, adduction, internal rotation, and external rotation. Note any limitations, pain, or compensatory movements. Compare the affected side to the unaffected side. Passive range of motion (PROM) is then assessed, with the examiner moving the patient’s arm through its range. Compare AROM and PROM; discrepancies may indicate capsular tightness or muscle weakness. Measure the range of motion using a goniometer for objective quantification. Internal and external rotation should be assessed with the elbow flexed to 90 degrees. Document the range of motion in degrees for each movement. Note any pain experienced during the movements. Assess for any crepitus or clicking during the range of motion assessment. The presence of pain or limitations in specific movements can provide clues to the underlying pathology. For example, limited abduction might suggest rotator cuff pathology, while pain during external rotation may point towards infraspinatus involvement. A thorough ROM evaluation is essential for comprehensive shoulder assessment.
IV. Provocative Tests for Impingement
Several provocative tests help identify subacromial impingement. The Neer impingement test involves passively flexing the patient’s shoulder to 160 degrees while internally rotating the humerus. Pain elicited suggests subacromial impingement. Hawkins-Kennedy impingement test involves flexing the shoulder to 90 degrees, then internally rotating the humerus and flexing the elbow. Pain indicates potential impingement; The painful arc test assesses pain during abduction between 60 and 120 degrees, which is a characteristic sign of impingement. The empty can test assesses supraspinatus function by having the patient abduct their arms to 90 degrees, internally rotate the shoulders, and extend their thumbs downward, then resist downward pressure. Weakness or pain suggests supraspinatus pathology, often related to impingement. The lift-off test assesses subscapularis function. The patient attempts to lift their hand off their back. Inability to do so suggests a subscapularis tear, which may contribute to impingement. Accurate interpretation of these tests requires careful attention to the patient’s response and the examiner’s technique. Remember to compare findings between the affected and unaffected shoulder. Positive results from these tests should be interpreted in the context of the patient’s history and other physical examination findings.
V. Rotator Cuff Tests
Several tests assess the integrity of the rotator cuff muscles. The empty can test, previously described in impingement testing, also evaluates the supraspinatus, a key rotator cuff muscle. Weakness or pain during this test suggests supraspinatus pathology. The drop arm test assesses the integrity of the rotator cuff, particularly the supraspinatus. The patient abducts their arm to 90 degrees; if they cannot slowly lower it, it suggests a rotator cuff tear. The external rotation lag sign assesses the infraspinatus and teres minor muscles. The examiner passively externally rotates the patient’s shoulder; inability to maintain this position suggests weakness or tear. The internal rotation lag sign assesses the subscapularis. The patient internally rotates their arm; if unable to maintain the position, subscapularis pathology is suspected. The lift-off test, also mentioned earlier, evaluates the subscapularis. The patient is asked to lift their hand from their back. Failure to do this indicates subscapularis weakness. These tests should always be compared with the unaffected side for accurate assessment. The results are interpreted considering the patient’s history and findings from other parts of the shoulder examination. Positive findings need further investigation to confirm a diagnosis and rule out other potential pathologies.
VI. Labral Tear Tests
The labrum, a ring of cartilage surrounding the glenoid, can be assessed through several specific maneuvers. The apprehension test, for anterior labral tears, involves passively abducting and externally rotating the patient’s shoulder. A positive test elicits apprehension or pain, suggesting instability and a potential anterior labral tear. The relocation test follows the apprehension test; applying pressure over the anterior aspect of the humeral head during the apprehension maneuver alleviates the apprehension or pain, supporting the diagnosis of anterior instability. The crank test, another useful test for labral tears, involves axial loading and rotation of the humerus. A positive finding is pain or a click, indicating a possible labral lesion. The anterior slide test assesses the anterior labrum. The examiner applies an anterior force to the humeral head while the shoulder is in abduction and external rotation. Pain or a click suggests a labral tear. The posterior labrum can be assessed with the posterior apprehension test, similar to the anterior apprehension test but with internal rotation. Remember that these tests are not definitive and should be interpreted alongside other clinical findings and imaging studies. A combination of positive labral tests, coupled with a detailed history and other examination findings, increases confidence in diagnosing a labral tear.
VII. Stability Tests
Evaluating shoulder stability involves assessing the integrity of the glenohumeral joint’s supporting structures – ligaments, tendons, and muscles. Several tests help determine the presence of instability. The apprehension test, while also used for labral tears, assesses anterior instability by passively abducting and externally rotating the arm; apprehension or pain suggests potential instability. The relocation test follows, applying anterior pressure to the humeral head, relieving apprehension if present. The sulcus sign evaluates inferior instability; traction is applied to the arm, creating a sulcus below the acromion process if inferior instability exists. The load and shift test assesses anterior and posterior instability. With the shoulder abducted to 90 degrees, the examiner applies an anterior and then posterior force to the humeral head, observing the degree of translation. Excessive translation indicates instability. The jerk test evaluates multidirectional instability; the arm is passively abducted and externally rotated, then the examiner applies an axial load. A sudden jerk or clunk suggests instability; These tests, although helpful, need to be correlated with patient history, other examination findings, and imaging studies for a definitive diagnosis of shoulder instability.
VIII. Special Tests for Biceps Pathology
The biceps tendon, traversing the shoulder joint, is susceptible to various pathologies, including tendinitis, tears, and subluxation. Several special tests help identify these conditions. Yergason’s test assesses for biceps tendon instability by resisting supination and elbow flexion while palpating the bicipital groove; pain or a palpable “pop” suggests pathology. Speed’s test evaluates biceps tendinitis; resistance is applied to elbow flexion and shoulder abduction with the forearm supinated; pain indicates a positive test. The active compression test (O’Brien’s test) differentiates between superior labral anterior-posterior (SLAP) lesions and biceps tendinitis. The patient flexes the shoulder to 90 degrees, internally rotates the arm, and then extends and resists downward pressure on the forearm; pain suggests biceps pathology, and relief of pain with supination suggests SLAP lesion. Finally, the painful arc test reveals pain during shoulder abduction between 60-120 degrees, often indicative of biceps tendinitis or subacromial impingement. These tests, in conjunction with clinical presentation and imaging, guide the diagnosis and management of biceps tendon pathologies.
IX. Neurological Examination
A comprehensive shoulder examination necessitates a neurological assessment to rule out nerve involvement. The brachial plexus, comprising nerves originating from the cervical spine, innervates the shoulder and upper limb. Assess sensory function by testing light touch, pinprick, and temperature sensation in the dermatomes supplied by the axillary, musculocutaneous, radial, median, and ulnar nerves. Motor function evaluation involves assessing strength of muscles innervated by these nerves—deltoids (axillary), biceps (musculocutaneous), triceps (radial), wrist flexors/extensors (median/radial/ulnar), and finger flexors/extensors (median/ulnar). Observe for any muscle atrophy or fasciculations. Deep tendon reflexes, including biceps, triceps, and brachioradialis, are tested to detect any abnormalities. The presence of paresthesia, numbness, weakness, or altered reflexes may indicate nerve root compression, peripheral nerve injury, or other neurological conditions, necessitating further investigation. Thorough documentation of neurological findings is crucial for accurate diagnosis and treatment planning.
X. Imaging Considerations
Imaging plays a crucial role in confirming the diagnosis following a thorough physical examination. Standard radiographs, including anteroposterior, lateral, and axillary views, are typically the initial imaging modality. These provide information on bony structures, identifying fractures, dislocations, arthritis, or osteophytes. However, radiographs may not visualize soft tissue structures effectively. If soft tissue pathology is suspected, such as rotator cuff tears, labral tears, or tendonitis, advanced imaging techniques are necessary. Magnetic resonance imaging (MRI) offers superior soft tissue contrast, providing detailed visualization of muscles, tendons, ligaments, and cartilage. MRI arthrography, involving intra-articular injection of contrast material, enhances visualization of labral tears and other intra-articular pathologies. Ultrasound, a readily available and cost-effective technique, can evaluate soft tissue structures, assess tendon integrity, and guide injections. Computed tomography (CT) scans are less frequently used in routine shoulder evaluations but are helpful for evaluating complex fractures or assessing bone pathology.
XI. Differential Diagnosis
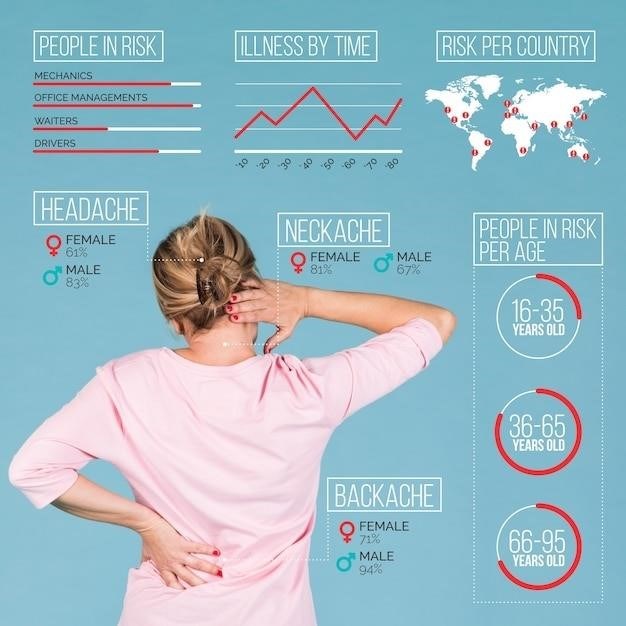
Establishing an accurate diagnosis for shoulder pain requires a systematic approach to differentiate among various conditions. The differential diagnosis should consider a broad range of possibilities, including rotator cuff tears (supraspinatus, infraspinatus, teres minor, subscapularis), labral tears (SLAP lesions, Bankart lesions), acromioclavicular joint (AC) osteoarthritis or separation, subacromial impingement syndrome, adhesive capsulitis (frozen shoulder), glenohumeral instability (anterior, posterior, multidirectional), biceps tendinopathy, and cervical radiculopathy. Thorough history taking, focusing on the mechanism of injury, location and character of pain, and associated symptoms, is essential. Careful physical examination, including assessment of range of motion, palpation for tenderness, and performance of specific provocative tests, helps narrow the differential. The combination of patient history, physical findings, and imaging results guides the clinician towards the most likely diagnosis. Referral to a specialist, such as an orthopedist or physiatrist, may be necessary for complex cases or when imaging findings are inconclusive.
XII. Documentation and Reporting
Meticulous documentation of the shoulder examination is crucial for effective communication and continuity of care. The report should include a comprehensive history detailing the patient’s chief complaint, mechanism of injury (if applicable), pain characteristics (location, severity, duration, radiation), and any relevant medical history. A detailed description of the physical examination should follow, noting findings from inspection (e.g., asymmetry, atrophy, swelling), palpation (e.g., tenderness, crepitus), range of motion (ROM) measurements (active and passive), and results of specific provocative tests (e.g., Neer, Hawkins-Kennedy, Empty Can, Yergason). The assessment section should synthesize the findings, offering a concise summary of the likely diagnosis and its severity. A clear plan, outlining management strategies (e.g., conservative treatment, physical therapy, surgical intervention), should be detailed. Finally, the report should include any referrals made to other specialists and a prognosis based on the anticipated recovery timeframe and functional outcomes. Using standardized forms and terminology ensures clarity and facilitates efficient communication among healthcare professionals.